News & Publications
Melanoma In Situ Excision Guidelines
June 1, 2013
By Alden R. Webb, D.O.
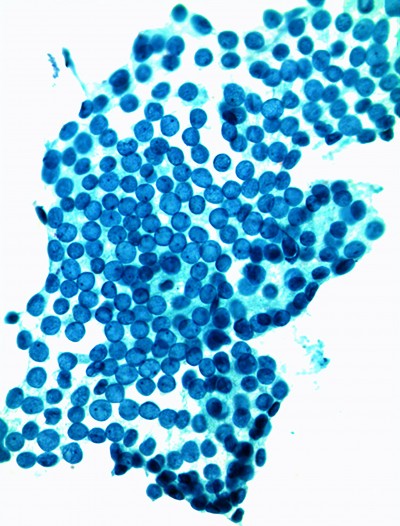
Recommendations for setting the appropriate margins when excising melanoma in situ (MIS) lesions are being revisited. A recent study1 published in the March 2012 Journal of the American Academy of Dermatology disclosed that larger skin margins provided a significantly higher success rate in a widespread test pool. The minimal surgical margin used in the study was 6 mm (more than the recommended 5 mm), and the total margin was subsequently 9 mm. All of these lesions were excised using Mohs micrographic surgery.
In the above mentioned study, the minimal surgical margin of 6 mm effectively removed 86% of the tumor, whereas a 9-mm margin removed 98.9%. With these results, it could be argued that 9 mm becomes the standard of care. It should also be mentioned that the published study did not consider margins less than 6 mm because the primary study site was a referral center, and the tumors were frequently treated prior to presentation at the clinic.
Surgical excision is still the standard treatment for most melanomas. The majority of patients only need 1 cm of normal-appearing tissue surrounding the lesion to be removed when detected early, because thin tumors have usually not spread beyond the original site. This procedure can be completed in a physician’s office with simple outpatient surgery. The cosmetic effect is minimal, and the patient can return to normal lifestyle activities immediately.
Twenty years ago, a National Institutes of Health Consensus Conference determined that a 5-mm surgical margin was the “standard of care” treatment for MIS. In the years following these guidelines, published data exposed the need for wider margins in instances of larger diameter lesions and some lesions in the head and neck area.
In 2008, a correlation between lesion diameter and surgical margin was made. The National Comprehensive Cancer Network maintained that a 5 mm margin is appropriate for MIS, with the following exceptions: larger MIS lesions and lentigo maligna types. In these instances, larger surgical margins may be necessary. The lesion’s subtype, location, and diameter should help the surgeon determine the appropriate margin for each case.
Ideally, every surgeon (and patient) wants clean margins on the "rst attempt. The discovery of positive margins can cause additional anxiety for the patient and will more than likely result in additional tissue removal on a subsequent visit, because the positive margin may be generally unknown. Frequently, this happens in cosmetically sensitive areas like the head and neck, where tissue-sparing technique is valuable to maximize cure rate and minimize scarring.
Adoption of the 9-mm rule may well reduce the need for additional surgery and minimize stress, anxiety, expense, and inconvenience for the patient and his/her family. However, adoption of this benchmark is not a black-and-white decision. Many factors need to be considered, and each case is different. Excision of MIS has been characterized as more art than science, and based on what is involved, that statement seems more and more true.
References:
1 Kunishige JH et al. Surgical margins for melanoma
in situ. J Am Acad Dermatol 2012 Mar;66:438-44.