News & Publications
Incyte Diagnostics Adopts ToGA Guidelines: Gastric and Esophageal Adenocarcinoma Testing for HER2 Status - IHC vs. FISH
June 22, 2012
In 2012, more than 13,000 men and 8,000 women in the United States will be diagnosed with gastric adenocarcinoma, and 10,000 people will die from the cancer according to the National Cancer Institute. In addition, 16,500 people will be diagnosed with esophageal cancer resulting in 14,000 deaths this year. The majority of these esophageal cancers are adenocarcinomas and originate in the distal esophagus, at or near the junction with the stomach (gastroesophageal junction). The incidence of esophageal adenocarcinoma is increasing one percent per year and is believed to be due to the increasing incidence of gastroesophageal reflux disease (GERD).
Early stomach and esophageal adenocarcinomas often do not present symptomatically until the disease is well established. As a result, the patient is already in an advanced stage upon diagnosis. This fact alone underlies the importance of identifying a biomarker to assist in both predictive and prognostic applications.
There is growing evidence that Human Epidermal Growth Receptor-2 (HER2) is, in fact, an important biomarker and key driver of tumor growth in some gastric and esophageal adenocarcinomas. Studies have shown amplification of the HER2 gene or overexpression of the HER2 molecule occurs in about 20-30% of patients with gastric and esophageal adenocarcinoma.
The prognostic and predictive power of HER2 gene overexpression in breast cancer has been well established and guidelines for evaluating HER2 status were recently published. Recent evidence suggests that trastuzumab (Herceptin), a monoclonal antibody that targets HER2, in combination with chemotherapy, is a therapeutic option in patients with HER2-positive advanced gastric or esophageal adenocarcinoma.
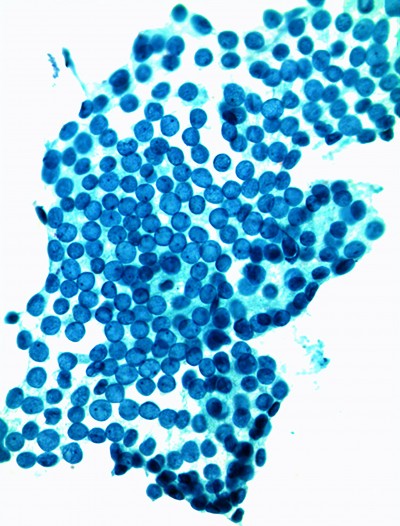
Over the past ten years, publications have shown that a HER2-positive status measured by immunohistochemistry (IHC) or in-situ hybridization (ISH) provides prognostic information related to survival or to relevant clinicopathologic characteristics of gastroesophageal adenocarcinoma. This includes established prognostic factors such as serosal invasion and lymph node metastases. There is clearly a potential role for HER2 as a negative prognostic factor in gastric and esophageal adenocarcinoma. From 2005 to 2010, an open-label, controlled trial evaluated the effect on overall survival of trastuzumab in combination with chemotherapy compared to chemotherapy alone in patients with HER2-positive advanced gastric cancer. The ToGA (Trastuzumab for Gastric Cancer) trial chose 594 patients from 24 countries with gastric or esophageal adenocarcinoma whose tumors showed overexpression of HER2 protein by immunohistochemistry or gene amplification by fluorescence in-situ hybridization (FISH).
From the very beginning of the ToGA trial, two important questions needed to be addressed from a biomarker perspective:
- Which analytical methods should be used for HER2 assessment?
- What would be the scoring criteria for biomarker analysis and associated inclusion algorithms?
The ToGA trial provided the largest group for HER2 testing in gastric cancer. It demonstrated that HER2 is a predictive biomarker for treatment with trastuzumab in gastric cancer, and that the applied scoring criteria are suitable for the selection of patients that benefit from trastuzumab. Since trastuzumab, in combination with chemotherapy, is becoming the standard of care in gastric cancer, appropriate patient selection by HER2 IHC and ISH testing is becoming a part of routine pathology for this disease.
The Food and Drug Administration recently approved trastuzumab for treatment of metastatic gastric and gastroesophageal cancer, based on the ToGA data. Results demonstrated a 2.7 month survival benefit of trastuzumab plus chemotherapy in HER2-positive advanced gastric and gastroesophageal adenocarcinoma, as compared with chemotherapy alone.
| Immunohistochemistry | ||
|---|---|---|
| Surgical specimen staining pattern | biopsy specimen staining pattern | HER2 overexpression assessment |
| 0 No reactivity or membranous reactivity in <10% of tumor cells | No reactivity in any tumor cell | Negative |
| 1+ Faint or barely perceptible membranous reactivity in 10% or more of tumor cells; cells are reactive only in part of their membrane. | Tumor cell cluster* with faint or barely perceptible membranous reactivity irrespective of percentage of tumor cells stained | Negative |
| 2+ Weak to moderate complete, basolateral or lateral membranous reactivity in 10% or more of tumor cells | Tumor cell cluster* with weak to moderate complete, basolateral or lateral membranous reactivity irrespective of percentage of tumor cells stained | Equivocal** |
| 3+ Strong, complete, basolateral or lateral membranous reactivity in 10% or more of tumor cells. | Tumor cell cluster* with strong complete, basolateral or lateral membranous reactivity irrespective of percentage of tumor cells stained | Positive |
|
* "tumor cell cluster" is defined as a cluster of 5 or more tumor cells |
||
|
Fluorescent in situ hybridization | ||
| HER2: Cep 17 Ratio |
Interpretation |
Criteria |
| <2.0 | Negative | Count at least 20 cells; survey for areas of highest gene count |
| ≥2.0 | Positive |
Count at least 20 cells; survey for areas of highest gene count. |
| At present, there is no equivocal category for HER2 FISH in gastric or gastroesophageal carcinoma, however, Ruschoff recommends counting additional cells if ratio near 2.0 (1.8-2.2) | ||
Analysis of the ToGA pathologic material showed that strong basolateral HER2 membrane staining by IHC correlates with HER2 amplification by FISH. Additionally, gastric and gastroesophageal carcinoma has a greater tendency toward HER2 heterogeneity as compared with breast carcinoma.
Consensus recommendations for gastric and gastroesophageal HER2 scoring (Table 1) have been established as a result of this data. These recommendations differ from breast cancer scoring. In gastric and gastroesophageal carcinoma, basolateral (incomplete) membrane staining is scored, and circumferential staining is not required. For biopsy specimens, amplification or strong basolateral staining in a small cluster of cells is reported as positive, while the 10% threshold is maintained for resection specimens.
| Tumor type/location | % HER2 positive |
|---|---|
| Gastric adenocarcinoma | 20.9% |
| Diffuse gastric (signet ring) carcinoma | 6.1% |
| Gastroesophageal junction adenocarcinoma | 33.2% |
| Overall ToGA | 22.1 % |
The ToGA studies have provided useful benchmarks regarding expected rates of positivity (Table 2) and have highlighted technical and interpretive pitfalls, including antibody reactivity with benign gastric epithelium and occasional strong cytoplasmic staining precluding interpretation.
One ToGA subgroup analysis found that HER2 FISH amplified but IHC-negative cases derive little benefit from trastuzumab, while the survival benefit excluding these cases was longer by over four months. Since trastuzumab in combination with chemotherapy is becoming the standard of care in gastric cancer, appropriate patient selection by HER2 IHC and ISH testing will now be part of routine pathology. Recommendations include having all patients HER2 tested at the time of initial diagnosis.
At Incyte Diagnostics, we have adopted the ToGA guidelines. We will test a patient’s first biopsy with IHC for HER2 with re!ex to ISH (FISH or CISH) for equivocal HER2 by IHC results. Since gastric and esophageal adenocarcinomas can be heterogeneous in HER2 overexpression or gene amplification, we recommend repeat HER2 testing on any subsequent resection specimen.