News & Publications
Good Smears Equal Good Medicine
June 1, 2013
By Ayumi I. Corn, M.D.
The handling and evaluation of bone marrow specimens have significantly evolved in the last several decades, due in large part to the increasing complexity of making a hematologic diagnosis. It is now common to evaluate cases for morphologic changes in conjunction with additional specialized testing, including flow cytometric, FISH, cytogenetic, and molecular analyses. Nationwide, there are differing trends in who performs the bone marrow biopsy. Currently, a wide variety of medical personnel performs the procedure, including hematology-oncology specialists, pathologists, physician assistants, nurses, and nurse practitioners. One thing that remains unchanged, however, is the importance of good specimen preparation.
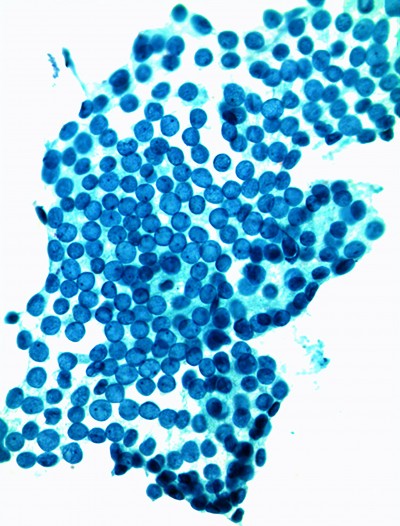
Accurate interpretation of bone marrow specimens is highly dependent on two factors: the quality of the sample obtained during the procedure and the quality of specimen processing, in particular the preparation of the bone marrow aspirate smears. Sometimes a good aspirate specimen may not be able to be obtained due to factors such as bone marrow fibrosis, a “packed” marrow, or technical difficulties, but in most situations, the quality of the prepared aspirate smears has a large impact on the ability of the pathologist to make a diagnosis.
There are two general options for preparing aspirate smears - either during the bone marrow procedure or after the procedure has been completed. Preparing slides during the procedure at the bedside requires multi-tasking and rapid handling of the specimen before clotting takes place. The result is a short window of time during which smears must be prepared and additional samples placed in anticoagulant tubes for ancillary studies. The advantage of properly made smears from a fresh aspirate specimen is that they can produce excellent cell morphology for evaluation by the pathologist.
The other option is to prepare the aspirate smears after the procedure has been completed. During the procedure, a portion of the aspirate specimen is placed in an EDTA anticoagulant tube (and mixed well) for this purpose. Then afterwards, the aspirate smears may be prepared at a less hurried pace. The advantage to this method is that one has more time to prepare the slides; a disadvantage is that a delay in slide preparation can lead to degenerative changes in the bone marrow cells. With either of the two methods, developing good technique in slide preparation requires training and plenty of experience. It is also helpful to have touch imprints of the core biopsy in cases with a poor aspirate specimen or a “dry tap.”
The quality of aspirate smears is a critical component in establishing a pathologic diagnosis. There are cell abnormalities that can only be detected on aspirate smears, such as in myelodysplastic syndromes, and this evaluation requires well-prepared and well-stained aspirate smears. Because the abnormalities detected on aspirate smears are not visible in core biopsies or clot sections, a bone marrow evaluation is incomplete without good aspirate smears.
Conversely, other disease processes are better represented in core biopsies, such as focal involvement of the bone marrow by lymphoma. A thorough evaluation of a bone marrow specimen by a pathologist requires both components and the ability to correlate the bone marrow findings with a peripheral blood smear.
Many factors influence the overall quality of a bone marrow specimen, and certainly not all biopsies will be optimal for evaluation by the pathologist. The preparation of good aspirate smears is an important step in this process, and the end result of a good bone marrow specimen is a timely and accurate diagnosis for the patient.