News & Publications
BRAF Mutation in Metastatic Melanoma
March 1, 2012
By David C. Hoak, M.D.
Until recently, a diagnosis of metastatic melanoma was often accompanied with a poor prognosis for treatment. Very little success had been achieved by a regimen of existing therapies until the discovery of the significant role played by the gene encoding kinase B-Rapidly Accelerating Fibrosarcoma (BRAF) in the growth and spread of this disease. This bleak outlook has brightened with new advancements in treatments for patients with BRAFV600E mutation-positive unresectable or metastatic melanoma.
Metastatic melanoma has been a highly invasive, fast-growing malignancy with few approved treatments available. Until recently, the two most commonly used therapies, high-dose interleukin-2 and dacarbazine, had response rates of only 10-20% and an even smaller percentage of complete responses. Dacarbazine (DTIC) was approved in 1970 and Interleukin-2 (IL-2) was approved by the FDA in 1998. Neither drug is thought to improve overall survival and in randomized trials, the median survival among patients treated with dacarbazine was less than eight months.
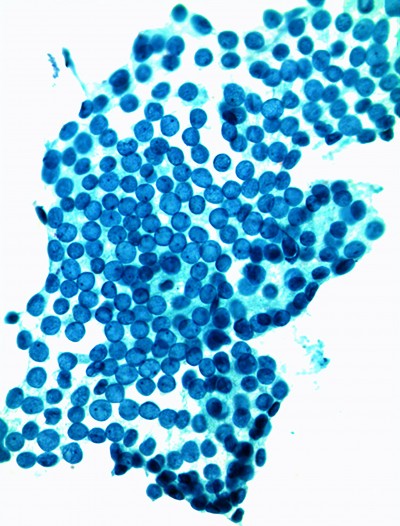
Research efforts looking for mutations in a large panel of common cancers revealed that 40-60% of melanomas and 7-8% of all cancers carry an activating mutation in the BRAF gene. A mutation in a gene can help some melanoma tumors grow and spread. People who have melanomas with a mutation in the BRAF gene have what is called a BRAF mutation-positive status. Research has shown that about half of all melanomas have the BRAF mutation.
BRAF mutations are also found in 40-70% of papillary or anaplastic thyroid cancers and in a small percentage of several other types of tumor. A large percentage (90%) of reported BRAF mutations result in the V600E mutation.
 The identification of mutations in the BRAF gene in the majority of melanomas offers an opportunity to test oncogene targeted therapy for this disease. A potent inhibitor of BRAF with the V600E mutation could provide an effective response to treating patients with metastatic melanoma.
The identification of mutations in the BRAF gene in the majority of melanomas offers an opportunity to test oncogene targeted therapy for this disease. A potent inhibitor of BRAF with the V600E mutation could provide an effective response to treating patients with metastatic melanoma.
BRAF plays an important role in both normal and cancer cells. Normally, BRAF protein is part of a chain of molecules relaying signals that tell cells how to grow and divide. This process is important for the cells in your body to function properly. A mutation in the BRAF gene can alter the way this protein works.
Instead of waiting for its turn to signal a cell to divide or grow, an altered BRAF signals all of the time. Out-of-control BRAF signaling may drive the uncontrolled growth of cancer cells. A drug that can target these mutated BRAF proteins, may slow down the growth of metastases.
The BRAF mutation-positive status of melanoma can be detected by diagnostic tests. If a patient is diagnosed with metastatic melanoma, testing for the BRAF mutation may be significant. Treatment of metastatic melanoma with oncogene targeted therapy in patients with tumors that carry the V600E BRAF mutation can result in complete or partial tumor regression in the majority of patients.
Melanomas can be categorized by specific molecular changes that drive the inhibition of the activated pathway in the individual tumors, leading to tumor regression. Recent trials have shown that therapies targeting tumors containing V600E BRAF mutations can induce complete or partial tumor regression in patients. Responses have been observed at all sites of disease, including bone, liver and small bowel.
Approximately 50% of melanomas harbor oncogenic BRAF mutations at position V600. Testing for the BRAFV600E mutation may help identify metastatic melanoma patients who may be appropriate candidates for vemurafenib (Zelboraf), a BRAF inhibitor therapy.
Although melanoma that has spread to distant sites is rarely curable, vemurafenib has demonstrated an improvement in progression-free survival (PFS) and overall survival (OS) in international, multicenter, randomized trials in patients with unresectable or advanced disease, resulting in U.S. Food and Drug Administration (FDA) approval in 2011. Vemurafenib is a selective BRAFV600E kinase inhibitor, and its indication is limited to patients with unresectable or metastatic melanoma with a demonstrated BRAFV600E mutation.